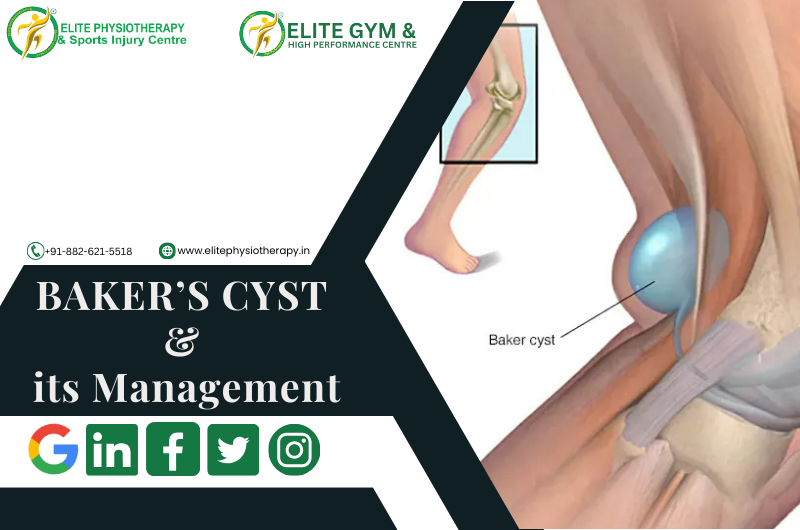
Baker’s cyst, sometimes called a popliteal cyst, is a swelling behind the knee filled with fluid. It happens when synovial fluid builds up in the popliteal bursa, a little sac that lessens friction between the tissues around the knee joint. Although Baker’s cyst is usually not fatal, it can be extremely uncomfortable and restrict physical activity, particularly in athletes and athletic people.
Our specialty at Elite Physiotherapy and Sports Injury Centre is diagnosing and treating Baker’s cysts using advanced modalities and Evidence-based physiotherapy procedures to guarantee the best possible outcome.
Causes of Baker’s Cyst
Usually, an underlying knee condition leads to Baker’s cyst forming. Typical reasons include:
- Osteoarthritis in the knee
- Rheumatoid arthritis.
- Meniscal tears
- Damage to cartilage
- Overuse injuries or trauma
For instance, a meniscal tear sustained by an elite athlete who jumps a lot could result in increased production of synovial fluid and the development of a Baker’s cyst.
Mechanism of Injury
When the knee joint becomes inflamed or irritated, too much synovial fluid is produced, which leads to the formation of the cyst. Through a one-way valve, this fluid escapes into the popliteal bursa. The bursa swells and develops into a palpable cyst behind the knee over time.
Signs, Symptoms, and Clinical Features of Baker’s Cyst
The following are Key symptoms of a Baker’s cyst:
- Tightness and swelling behind the knee
- Pain that gets worse when you flex your knees or stand for a long time
- Knee with limited range of motion (ROM)
- A bulge in the popliteal region that is felt or apparent
- Discomfort or stiffness during exercising
In extreme situations, the cyst may burst, allowing fluid to seep into the calf and producing symptoms similar to deep vein thrombosis (DVT), including redness, swelling, and warmth.
Diagnostic Methods at Elite Physiotherapy
At Elite Physiotherapy and Sports Injury Centre, we employ a combination of physical and functional assessments to diagnose Baker’s cysts effectively.
Physical Assessment:
- Check for obvious edema in the popliteal area.
- palpation to determine the cyst’s presence and size.
Special Physiotherapy Tests for Baker’s Cyst:
- The Bounce Home Test: Evaluates the knee joint’s integrity and detects any mechanical obstruction or effusion.
- McMurray’s Test: Assesses meniscal damage that could be a factor in the development of cysts.
- Apley’s Test: Assists in determining meniscal or ligamentous involvement.
- Modified Thompson Test: In order to rule out other diseases like DVT, this test looks for fluid leaking into the calf.
Functional Assessment:
- Examination of Gait patterns.
- Assessment of joint stability and muscle strength.
- To identify restrictions, use a range of motion testing.
Physiotherapy Management of Baker’s Cyst at Elite Physiotherapy
We treat Baker’s cysts using an individualized, evidence-based strategy that aims to minimize symptoms, enhance function, and stop recurrence. The cutting-edge treatments we provide are listed below:
1. Electrotherapy Modalities:
- Shock Wave Therapy: Promotes tissue regeneration, lowers inflammation, and eases popliteal discomfort.
- The Super Inductive System (SIS): Uses high-frequency electromagnetic stimulation to improve muscle activation and lessen knee stiffness.
- High-Intensity Class IV Laser Therapy: Promotes the reabsorption of synovial fluid, reduces inflammation, and speeds up tissue recovery.
2. Hydrotherapy:
- In a regulated setting, water-based workouts improve muscular strength and mobility while lowering joint stress.
3. Cryotherapy:
- Localized cold therapy reduces pain and swelling, particularly after physical exercise.
4. Manual Therapy:
- Soft tissue mobilization to ease constriction around the popliteal region.
- Joint mobilization to increase knee range of motion.
5. Therapeutic Exercises for Baker’s Cyst:
- Stretching exercises: Stretches for the hamstrings and calves help release tension in the area surrounding the knee joint.
- Strengthening Exercises: To improve joint stability, concentrate on your quadriceps, hamstrings, and glutes.
- Proprioception and Balance Training: Enhancing knee control and preventing more injuries are two benefits of proprioception and balance training.
6. Taping Techniques:
- Kinesiology taping helps to ensure adequate alignment during exercises and lessens the pressure on the knee joint.
7. Progressive Rehabilitation Program:
- Designed to meet the needs of each participant, this program aims to gradually restore full function and resume daily activities or sports.
Why Choose Elite Physiotherapy for Baker’s Cyst?
Our team at Elite Physiotherapy and Sports Injury Centre is dedicated to providing top-notch care through individualized treatment plans and state-of-the-art technologies. In addition to providing symptom alleviation, our all-encompassing strategy guarantees the long-term avoidance of Baker’s cysts and related knee disorders. With access to cutting-edge techniques including hydrotherapy, shock wave therapy, and super inductive systems, we offer unparalleled proficiency in treating musculoskeletal disorders and sports injuries.
Speak with one of our experts now to start along the path to pain-free mobility and peak performance. Your recovery is our top concern at Elite Physiotherapy!