What is Posterior tibial tendonitis?
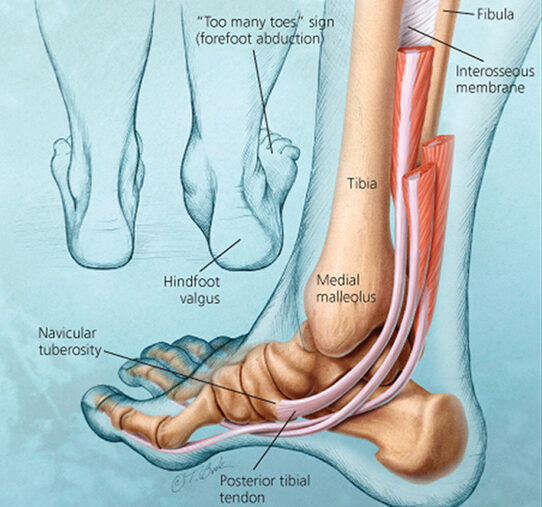
Posterior tibial tendonitis, or posterior tibial tendon dysfunction (PTTD), is a common condition impacting the foot and ankle. It occurs when the posterior tibial tendon becomes inflamed or damaged, impairing its ability to support the arch of the foot. It can give rise to an adult-acquired flatfoot deformity, resulting in pain and reduced mobility.
Causes and Mechanism of Injury
Posterior tibial tendonitis is frequently caused by overuse, especially in activities that put repetitive stress on the tendon, like running, hiking, or walking for extended periods. Obesity, hypertension, diabetes, and prior injuries to the foot or ankle are additional contributing factors. The posterior tibial tendon is essential for keeping the medial arch intact and enabling foot inversion. When this tendon is damaged, it may result in an arch collapse and the onset of a flatfoot deformity.
Signs and Symptoms
Individuals with Posterior tibial tendonitis may experience:
- Swelling and pain on the inner side of the ankle and foot.
- Flattening of the foot’s arch.
- Inward ankle rolling.
- Difficulty when trying to stand on tiptoe.
- Pain in the foot and ankle, particularly following exercise.
If these symptoms are not treated, they can worsen and result in major deformity and disability.
Diagnostic Methods at Elite Physiotherapy and Sports Injury Centre
At Elite Physiotherapy and Sports Injury Centre, we employ comprehensive physical and functional assessments to diagnose Posterior tibial tendonitis:
- Clinical Evaluation: Our physiotherapists perform detailed evaluations, monitoring foot posture, gait characteristics, and regions of sensitivity.
- Specialized Physiotherapy Tests: We employ targeted assessments to assess the condition of the posterior tibial tendon:
- Single-Leg Heel Raise Test: The patient tries to elevate onto the toes while balancing on one leg. If it is difficult or impossible to do this, it suggests dysfunction of the posterior tibial tendon.
- Palpation and Loading Test: Pain and structural integrity are evaluated by applying gentle pressure along the tendon while the foot bears weight.
Physiotherapy Management at Elite Physiotherapy and Sports Injury Centre
Our center offers a holistic approach to managing Posterior tibial tendonitis, focusing on non-surgical interventions tailored to each patient’s needs:
1. Activity Modification:
To avert additional strain on the tendon, we recommend cutting back on or modifying activities that worsen symptoms.
2. Orthotic Support:
Custom-made orthotics or ankle braces are supplied to support the medial arch and stabilize the foot, assisting in proper alignment during everyday activities.
3. Therapeutic Exercises:
A tailored exercise program is created to fortify the posterior tibial tendon and adjacent muscles, thereby improving foot stability and function. Below are key exercises included in our treatment approach:
- Strengthening Exercises
The purpose of these exercises is to regain strength in the posterior tibial tendon and adjacent muscles, which will lead to enhanced stability of the foot.- 1. Resisted Foot Inversion:
- Use a resistance band positioned around the foot.
- Gently rotate the foot inward while facing resistance.
- Do 3 sets of 10 reps for each foot.
- 2. Heel Raises (Double-Leg & Single-Leg):
- Position yourself on a level surface and elevate yourself onto your toes so that your heels are raised off the ground.
- Begin with your feet positioned together, then advance to raising one leg.
- Execute 3 sets of 15 reps.
- 3. Arch Doming Exercise (Short-Foot Exercise):
- While seated, attempt to elevate the arch of your foot without curling your toes.
- Maintain for 5 seconds, then ease up.
- Complete three sets of ten reps.
- 1. Resisted Foot Inversion:
- Flexibility & Mobility Exercises
To alleviate stress on the posterior tibial tendon, flexibility is essential.- 1. Calf Stretch (Stretching the Gastroc & Soleus):
- Position yourself so that you are facing a wall, with one foot advanced and the other extended back.
- To stretch the gastrocnemius, keep the back leg straight, and to stretch the soleus, bend the knee.
- Maintain each stretch for half a minute and do it three times for every leg.
- 2. Posterior Tibial Tendon Stretch:
- Rest your foot on the opposite knee while you sit.
- Gently stretch your foot outward with your hands.
- Maintain for 20–30 seconds, and do it three times for each leg.
- 1. Calf Stretch (Stretching the Gastroc & Soleus):
- Balance & Proprioception Training
Proprioceptive exercises are crucial due to the important function of the posterior tibial tendon in stabilizing the foot.- 1. Single-Leg Stance:
- Balance on one foot for half a minute, and as you improve, try shutting your eyes or using an unstable surface (like a balance board).
Do 3 sets for each leg.
- Balance on one foot for half a minute, and as you improve, try shutting your eyes or using an unstable surface (like a balance board).
- 2. Bosu Ball Training:
- To improve foot stability, do squats or maintain a single-leg stance on a Bosu ball.
Maintain for half a minute, and then replicate three sets.
- To improve foot stability, do squats or maintain a single-leg stance on a Bosu ball.
- 1. Single-Leg Stance:
4. Manual Therapy:
Our physiotherapists utilize methods like soft tissue mobilization and joint mobilization to enhance flexibility, alleviate pain, and bring back normal movement patterns.
- Soft Tissue Mobilization (STM)
- Targeted massage techniques break down adhesions, enhance blood circulation, and decrease inflammation in the posterior tibial tendon.
- STM also targets compensatory muscle tightness in the calves, plantar fascia, and peroneal muscles.
- Myofascial Release (MFR)
- A slow and sustained stretch relieves tension in the soft tissues surrounding the posterior tibial tendon.
- Helps in enhancing foot mobility and reinstating arch support.
- Joint Mobilization
- Talocrural & Subtalar Joint Mobilization: By improving ankle and foot mechanics, talocrural and subtalar joint mobilization lessens the load on the posterior tibial tendon.
- Midfoot Mobilization: The navicular and cuneiform bones are essential for preserving the foot arch.
- Active Release Technique (ART)
- In order to relieve tension and enhance movement patterns, the physiotherapist applies pressure to the tendon as the patient moves the foot.
- Dry Needling & Trigger Point Therapy
- To reduce discomfort and enhance muscle activation, dry needling targets trigger sites in the calf muscles and posterior tibial tendon.
5. High-End Modalities:
We use cutting-edge therapy technology to reduce symptoms and hasten healing:
- Shock Wave Therapy: Shock wave therapy uses acoustic waves to lessen pain and encourage tissue regeneration.
- Capacitive Resistive Electric Transfer (CRET) Therapy: Capacitive Resistive Electric Transfer (CRET) therapy uses targeted electromagnetic energy to improve deep tissue healing.
- Super Inductive System: Increases muscle strength and decreases pain by stimulating neuromuscular regions with high-intensity electromagnetic fields.
- High-Intensity Class 4 Laser Therapy: High-intensity Class 4 laser therapy delivers deeply penetrating light energy to stimulate tissue repair and reduce inflammation.
- Hydrotherapy: Hydrotherapy uses water exercises to increase strength and flexibility while minimizing joint stress.
- Cryotherapy: Uses cold therapies to ease pain and reduce inflammation.
Elite Physiotherapy and Sports Injury Centre guarantees a thorough and efficient treatment plan for patients with posterior tibial tendonitis by combining these cutting-edge technologies with conventional physiotherapy procedures.
Conclusion
Effective management of posterior tibial tendinitis depends on early diagnosis and treatment. To restore function and enhance our patients’ quality of life, we at Elite Physiotherapy and Sports Injury Centre are dedicated to offering individualized care using both traditional and innovative methods.

