Introduction
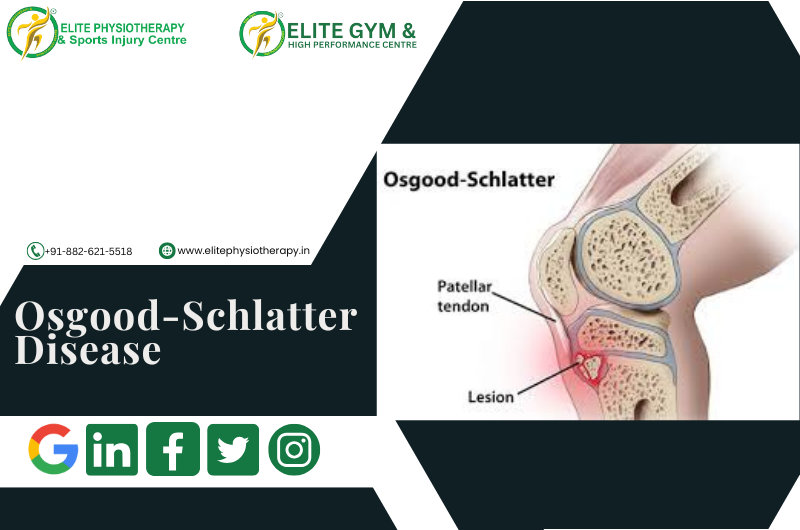
Osgood-Schlatter Disease (OSD) Usually occurs between the ages of 10 and 15, It is a frequent overuse injury that mostly affects teenagers during their growth spurts. Repetitive strain on the patellar tendon, which joins the quadriceps muscle to the tibial tuberosity, causes this condition to occur. At the tibial tuberosity, where the tendon enters, prolonged traction of this tendon causes pain, inflammation, and maybe bone formation. Our specialty at Elite Physiotherapy and Sports Injury Centre is treating sports-related injuries, such as OSD, using a customized, athlete-centered approach to recovery and reconditioning.
Understanding Osgood-Schlatter Disease
Pathophysiology and Causes
The primary cause of OSD is repeated strain on the patellar tendon, which is made worse by young athletes’ fast development stages. Sports like basketball, track & field, and soccer that require a lot of jumping, sprinting, or sudden direction changes can cause microtrauma by putting stress on the tibial tuberosity. The underlying factors include:
- Rapid Growth Spurt: Adolescence’s rapid growth spurt causes strain at the bone-tendon contact because bones develop more quickly than muscles and tendons.
- Muscle Imbalance: Inflammation can result from weak or taut quadriceps and hamstrings that put more strain on the patellar tendon.
- Poor Biomechanics: The knee may be subjected to extra strain due to improper movement patterns, such as excessive foot pronation or knee valgus.
Symptoms
Osgood-Schlatter disease (OSD) often presents as localized pain and tenderness at the tibial tuberosity, which worsens with movement. Among the main symptoms are:
- Pain with Movement: Activities requiring knee extension, such jogging, jumping, kneeling, or climbing stairs, can make pain worse.
- Tenderness and Swelling: The tibial tuberosity may be painful, swollen, and occasionally noticeably larger.
- Pain Relief at Rest: Although more severe instances may cause ongoing pain, pain usually goes away when the person is at rest.
The history and clinical examination are the main factors used to make the diagnosis. Imaging (such as X-rays) can sometimes be performed to evaluate bone abnormalities in the tibial tuberosity or rule out other causes of knee discomfort.
Physiotherapy Management of Osgood-Schlatter Disease
At Elite Physiotherapy and Sports Injury Centre, Osgood-Schlatter disease management is personalized. Our evidence-based therapy programs are customized to match each patient’s symptoms, activity level, and functional goals. Here is the scientific approach we use:
Initial Assessment and Pain Management
To determine the severity and causes of OSD symptoms, our physiotherapists start with a comprehensive evaluation. The first aim is pain management:
- Activity Modification: We recommend that patients temporarily cut back on or alter high-impact sports like running, jumping, and other activities that make their discomfort worse.
- Ice Therapy: Several times a day, using ice packs for 10 to 15 minutes can help manage pain and inflammation.
- Bracing and Taping: In extreme situations, a knee brace or patellar tendon strap can relieve strain on the tendon and lessen the strain on the tibial tuberosity.
Stretching and Flexibility Exercises
To release tension in the muscles surrounding the knee joint, gentle stretching exercises are crucial. These workouts aim to:
- Quadriceps Stretch: Stretching the quadriceps lengthens them and lessens the strain on the patellar tendon. We make care to use the right method to prevent making problems worse.
- Hamstring Stretch: We include the hamstrings in the stretching regimen because they might have an indirect impact on knee mechanics.
- Calf Stretch: In order to maintain balanced flexibility, we include calf stretching since tight calves can change biomechanics and impact knee loads.
Strengthening Exercises
To stabilize the knee joint and enhance muscle balance surrounding the knee, strengthening activities are essential. We consist of:
- Strengthening the Quadriceps: Without putting undue pressure on the knee, exercises like wall sits, straight-leg lifts, and isometric contractions will help you progressively increase your quadriceps’ strength.
- Hip and Core Strengthening: We use exercises like clamshells, side-lying leg lifts, and planks because weak hip and core muscles can result in poor knee control.
- Strengthening of the Hamstrings and Glute: Exercises like squats, hamstring curls, and bridges can progressively added to improve overall knee stability.
Progressive Functional Training
We start with functional exercises that mimic motions found in sports after pain is under control and strength has increased. These exercises include:
- Dynamic Stretching and Agility exercises: Gradually, mini jumps, controlled lunges, and agility ladder exercises are added.
- Plyometric Training: To develop strength and endurance in a controlled way, gradually introduce low-impact plyometric exercises like box step-ups and hopping.
Neuromuscular Training and Biomechanics Correction
To prevent recurrence, it is essential to correct movement patterns and teach proper biomechanics. We highlight the following techniques:
- Training for Balance and Proprioception: Activities that promote neuromuscular control include single-leg stands, balance boards, and Bosu ball workouts.
- Gait and Running Mechanics: By evaluating running and jumping skills, we can, therefore, identify any biomechanical defects in young athletes.
Education and Injury Prevention Strategies
- Education on Self-Management
We teach patients and their families the value of regular stretching, appropriate warm-ups, and rest. Depending on pain levels and strength recovery, our physiotherapists, accordingly, provide at-home workout regimens and, furthermore, guidance on a gradual return to sports.
- Footwear and Orthotics
Wearing the right shoes can reduce knee strain, particularly for young athletes participating in high-impact sports. We evaluate whether orthotic insoles are necessary to improve knee alignment, particularly in cases of pronation or other biomechanical anomalies.
- Return-to-Play Guidelines
The return to play process at Elite Physiotherapy and Sports Injury Centre is methodical, with a focus on a gradual reintroduction to sport-specific drills and close observation of any pain or discomfort. Athletes should resume full activity only when they can perform everyday tasks and sporting activities without any pain.
Why Choose Elite Physiotherapy and Sports Injury Centre?
At Elite Physiotherapy and Sports Injury Centre, our staff, therefore, commits to offering young athletes with Osgood-Schlatter disease thorough and, most importantly, personalized care. Our strategy is based on cutting-edge rehabilitation methods, ongoing education, and sport-specific modifications since we recognize how important it is to keep athletes active and pain-free. By giving our young customers the resources they require for long-term knee health, we want to help them resume their sports with confidence and avoid further problems.
Conclusion
For young athletes, Osgood-Schlatter Disease can be a difficult disease, but recovery is possible with prompt diagnosis and suitable treatment. In order to guarantee a successful and long-lasting return to sport, we at Elite Physiotherapy and Sports Injury Centre place a strong emphasis on individualized care that gives priority to pain management, muscle balance, and functional training.
If your child or young athlete is experiencing knee pain or showing signs of Osgood-Schlatter disease, contact Elite Physiotherapy and Sports Injury Centre today to book a consultation with our expert team.