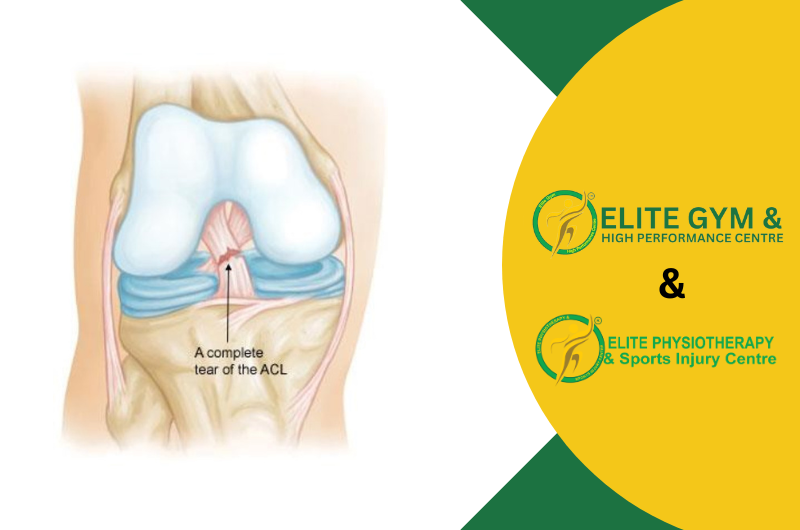
One of the main stabilizers of the knee joint is the Anterior Cruciate Ligament (ACL), which controls rotational stability and limits the tibia’s excessive forward motion in relation to the femur. ACL injuries are among the most frequent sports-related injuries, especially among athletes who play activities like football, cricket, basketball, skating, and weightlifting that require abrupt stops, direction changes, and jumping. To assist athletes and active people in their recovery, Elite Physiotherapy and Sports Injury Centre offers specialist, evidence-based treatment for ACL injuries.
Understanding ACL Injuries
The ACL is a strong band of tissue that connects the tibia (shinbone) and femur (thigh bone) inside the knee joint. It is essential for maintaining knee stability during pivoting, cutting, and leaping motions. An injury to the ACL can cause a variety of symptoms and limitations, such as:
- Sudden and intense pain Usually occurs as soon as an injury occurs, followed by swelling that happens quickly.
- A popping sensation: Many people claim to have heard or felt a “pop” at the scene of the injury.
- Instability: The sensation of the knee “giving way” when moving, particularly when twisting or pivoting.
- Stiffness and swelling: Stiffness and swelling can develop in a matter of hours, causing limited mobility and trouble bending or straightening the knee.
Diagnosis of ACL Injuries
Appropriate treatment requires an accurate diagnosis. Usually, the diagnostic procedure entails:
- Physical Examination: Specific tests that evaluate ligament integrity include the Lachman Test, Pivot Shift Test, and Anterior Drawer Test.
- MRI (Magnetic Resonance Imaging) is frequently used to discover related damage (such as meniscal tears, bone bruising, or damage to other ligaments), confirm the diagnosis, and assess the degree of the injury.
Management Approaches for ACL Injuries
Several variables, such as the severity of the injury, the patient’s age, activity level, and rehabilitation objectives, influence the decision between surgery and non-surgical treatment. A thorough analysis of both strategies is provided below:
Surgical Management
1. Surgical Indications
In general, surgery is advised for:
- People with total ACL injuries, particularly those who want to resume pivoting or high-impact sports.
- Those whose knee instability does not go away after therapy.
- Individuals with meniscal tears or other ligament damage in addition to their knee ailments.
2. Surgery: Reconstruction of the ACL
The most popular surgical technique is ACL repair, which includes:
- Graft Selection: Surgeons employ either allografts (donor tissue) or autografts (from the patient’s own body, usually from the hamstring or patellar tendon). Every graft type offers benefits, and the patient’s age, degree of activity, and preferences will determine the best for them.
- Arthroscopic surgery is a minimally invasive treatment that is guided using an arthroscope, which is a tiny camera. After removing the torn ACL, screws or other fixation devices are used to place and secure the new graft.
- Rehabilitation Protocol: To restore knee function, strength, and stability following surgery, rehabilitation is crucial.
3. Post-Surgical Rehabilitation Stages
We provide a systematic rehabilitation program at Elite Physiotherapy and Sports Injury Centre that is customized to meet the needs of each patient:
- Phase 1 (0–2 weeks post-op): Prioritize knee extension recovery, quad activation promotion, and pain and inflammation reduction. Manual treatment, cryotherapy, and mild range-of-motion exercises are used.
- Phase 2 (2–6 weeks): To enhance joint stability and muscle control, gradually move into weight-bearing activities and strengthening exercises such as heel slides, mini squats, and straight leg lifts.
- Phase 3 (6–12 weeks): Focus on functional and dynamic activities, such as teaching proprioception and balance using equipment like Bosu balls and wobble boards.
- Phase 4 (three to six months): Return to sports training, emphasizing plyometrics, agility exercises, and sport-specific drills to regain full function and get ready for safe
Non-Surgical Management
Non-surgical treatment may be a good choice for individuals with partial ACL injuries, minimal activity levels, or those who do not participate in high-impact sports. It consists of:
First Stage: Immobilization and Rest
To manage pain and swelling after an accident, rest and immobilization are crucial. During this stage, a knee brace may be utilized to offer support and stability.
Physiotherapy-Based Strengthening Program
A thorough physiotherapy program is essential for increasing stability and strength. Our main priorities at Elite Physiotherapy are:
- Strengthening the Hamstrings and Quadriceps: The stabilizing role of the ACL can be somewhat compensated for by strengthening these muscle groups. There are exercises like lunges, leg presses, and hamstring curls.
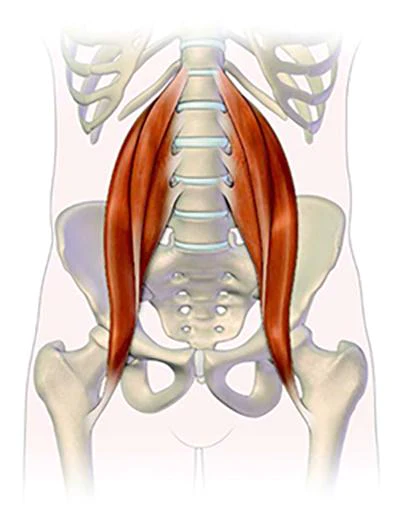
- Strengthening the hips and core: The stability of the knee is greatly influenced by the hip and core muscles. To make sure these muscles are strong and effective, we use exercises like planks, hip abductions, and bridges.
Proprioceptive and Balance Training
It is crucial to improve knee stability using proprioceptive exercises. We enhance neuromuscular control and coordination using single-leg exercises, Bosu balls, and balance boards.
Gradual Return to Activity
Patients are progressively reintroduced to functional exercises and sport-specific drills as their strength and stability increase. Our method guarantees that every stage of the progression is tailored to the recuperation and objectives of the individual.
Physiotherapy Management: A Comprehensive Approach at Elite Physiotherapy and Sports Injury Centre
Whether ACL injuries are treated surgically or non-surgically, physiotherapy is essential to the healing and rehabilitation process. Our team of skilled physiotherapists at Elite Physiotherapy creates customized rehabilitation plans to reduce the chance of re-injury while recovering function, strength, and mobility.
Rehabilitation Before Surgery (Prehab)
Physiotherapy before surgery focuses on:
- Lowering pain and swelling
- Getting back into range of motion
- Enhancing hip, hamstring, and quadriceps strength By ensuring that the knee is in optimal condition before surgery. Prehab enhances surgical results and expedites the healing process following surgery.
Physiotherapy Following Surgery
We break down our post-operative programs into distinct stages:
- Acute Phase: Electrical methods such as TENS (Transcutaneous Electrical Nerve Stimulation), manual therapy, and cryotherapy are used to manage pain and swelling.
- Progressive Strengthening Phase: To restore strength when discomfort and swelling have subsided, we incorporate more strenuous workouts including lunges, step-ups, and resistance band training.
- Advanced Functional Training: To get the player ready for a safe return to play, plyometric training, agility drills, and sport-specific workouts are employed. These programs are customized according to the sport and the unique requirements of the athlete’s position.
Prevention Programs
Elite Physiotherapy places a high premium on preventing re-injuries. Our programs for preventing ACL injuries include:
- Instruction on appropriate movement mechanics, such as landing and leaping methods
- Routines for strengthening and core stability
- Exercises for flexibility and agility to support healthy muscular growth
Conclusion
Because ACL injuries can be complicated, a thorough approach is necessary to guarantee a full recovery. Our mission at Elite Physiotherapy and Sports Injury Centre is to enhance athletic performance and recovery potential by offering patient-centered, evidence-based care. Our knowledgeable staff is dedicated to assisting you in regaining function, avoiding further injuries, and reaching your physical objectives, regardless of whether you are a top athlete or an active person.
For expert, individualized care if you have an ACL injury or would want more information about our ACL rehabilitation programs, contact Elite Physiotherapy and Sports Injury Centre. Allow us to accompany you on your path to recuperation and peak performance.