Incorrect alignment or frequent patella (kneecap) dislocation concerning the femoral groove (trochlea) is a complex problem known as patellofemoral instability. If left untreated, this condition may result in chronic joint degeneration, pain, and functional restrictions. Whether they are athletes, active people, or anybody else coping with patellofemoral issues, our goal at Elite Physiotherapy and Sports Injury Centre is to offer the best care possible.
Anatomy of the Patellofemoral Joint
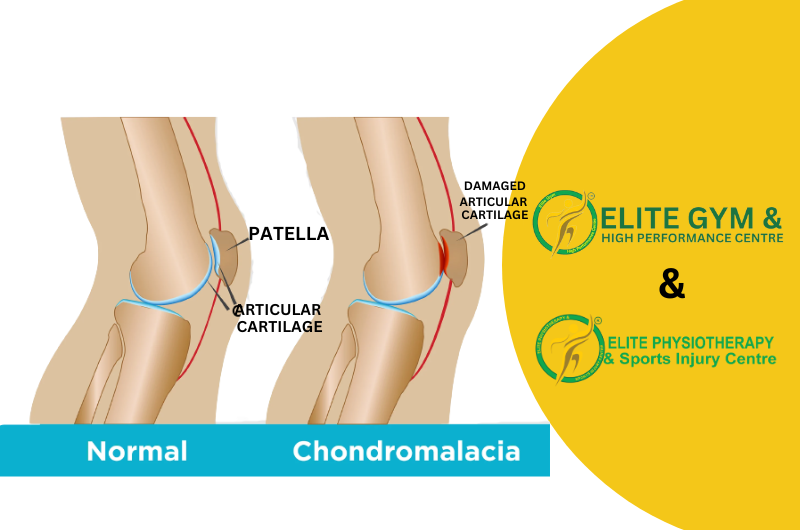
One of the knee’s essential parts is the patellofemoral joint. When walking, jogging, or kneeling, the patella moves smoothly inside the femur’s trochlear groove. Stability is preserved by:
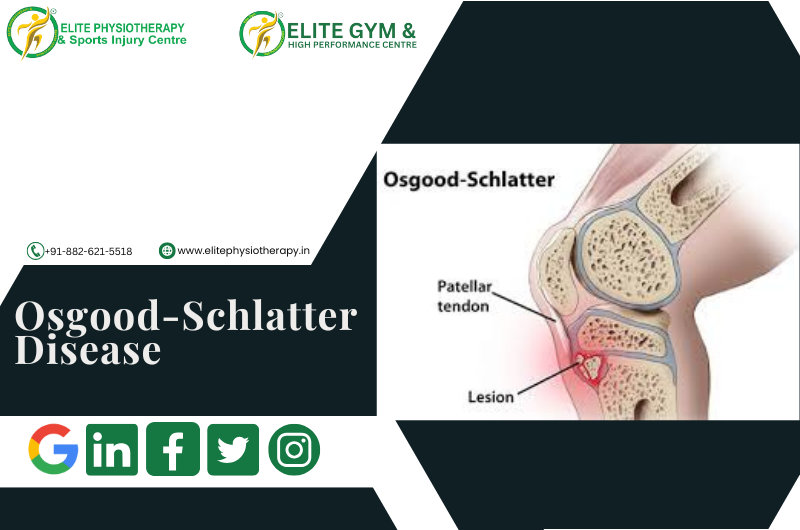
- Bony structures: The patella’s form and the depth of the trochlear groove.
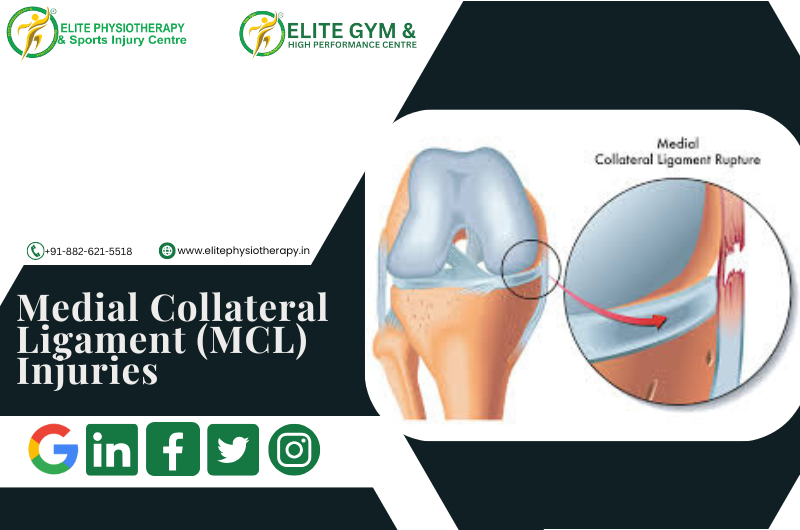
- Soft tissue restraints: The patellar tendon, quadriceps muscles, lateral retinaculum, and medial patellofemoral ligament (MPFL) are examples of soft tissue constraints.
When these components become disorganized or imbalanced, instability may result, which might cause the patella to move laterally or dislocate entirely.
Causes of Patellofemoral Instability
Traumatic Events: Patellar dislocation is frequently caused by direct strikes or twisting injuries.
Anatomical Predispositions:
- trochlear groove that is shallow.
- High-riding patella, or patella alta.
- The Q-angle, or the angle formed by the patellar tendon and quadriceps.
Muscle Imbalances:
- Weakness or delayed vastus medialis obliquus (VMO) activation.
- tight lateral structures, such as the lateral retinaculum or iliotibial band.
Ligamentous Laxity: People who have conditions like Ehlers-Danlos syndrome may be more prone to instability in the future.
Recurrent Dislocations: The patella is more vulnerable to instability in the future if it has been dislocated.
Symptoms of Patellofemoral Instability
Patients frequently arrive with:
- Knee Pain: Knee pain is mostly anterior and is worse when you squat or climb stairs.
- Instability: An unstable knee feels like it’s “giving way.”
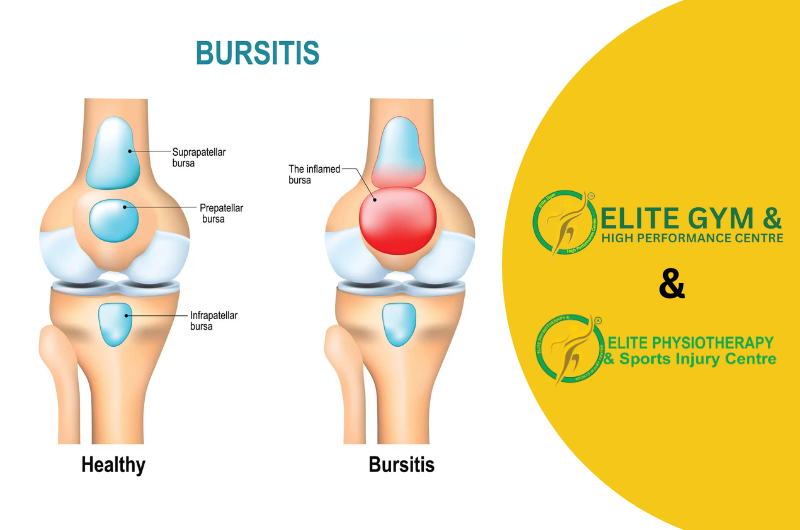
- Swelling: Particularly following a first displacement.
- Reduced Range of Motion: As a result of mechanical impediments or pain.
- Apprehension Sign: Fear or discomfort when the patella is moved laterally is an indication of apprehension.
Diagnosis
At Elite Physiotherapy and Sports Injury Centre, we evaluate patellofemoral instability using a variety of cutting-edge diagnostic techniques:
Clinical Assessment:
- Palpation to find effusion or discomfort.
- Special tests such as the J-sign observation, apprehension test, and patellar glide test.
Apart from our assessment, patellar instability can be diagnosed also by:
Imaging:
- X-rays: To evaluate trochlear morphology and bone alignment.
- MRI: For assessing soft tissues, such as cartilage degeneration and MPFL integrity.
- CT scans: To evaluate rotational alignment and measure patellar tilt.
Treatment Options
Non-Surgical Management
The first line of treatment is frequently non-surgical, particularly for people who have had only one dislocation or who have modest instability.
Physiotherapy:
The mainstay of treatment for patellofemoral instability is physiotherapy, which aims to enhance patellar tracking, stabilize the joint, and allow for a full return to function. We use a thorough and sophisticated approach at Elite Physiotherapy & Sports Injury Centre, combining manual therapy, therapeutic exercises, and state-of-the-art modalities.
Key Components of Physiotherapy Management
1. Management of Pain and Inflammation
- Cryotherapy: Using ice packs to minimize swelling and lessen pain.
- High-Intensity Laser Therapy (HILT): By promoting cellular regeneration, high-intensity laser therapy (HILT) speeds up tissue healing, lowers inflammation, and offers profound pain relief.
- Shock Wave Therapy: Shock wave therapy is useful for improving the repair of the soft tissues surrounding the patellofemoral joint and reducing chronic pain.
2. Soft Tissue and Joint Mobilization
Manual Therapy:
- Soft tissue mobilization: For tight lateral structures like the lateral retinaculum and iliotibial band, manual therapy involves mobilizing soft tissues.
- patellar mobilizations: To enhance trochlear groove alignment and gliding.
Cupping therapy: improves circulation and eases knee-related muscle strain.
3. Neuromuscular Activation and Muscle Strengthening
- To improve patellar tracking, the quadriceps should be strengthened, especially the vastus medialis obliquus (VMO).
- To improve total knee stability, progressive resistance training focuses on the calf, gluteal, and hamstring muscles.
- deep neuromuscular activation, which enhances muscle recruitment and decreases spasticity, through the use of advanced equipment like the Super Inductive System (SIS).
4. Stretching and Flexibility Training
- To ease tightness and encourage balanced patellar movement, perform stretches for the lateral structures, quadriceps, hip flexors, and iliotibial band.
- methods for increasing flexibility, such as Proprioceptive Neuromuscular Facilitation (PNF) stretching.
5. Proprioception and Balance Training
- To improve neuromuscular coordination and joint proprioception, use stability balls, wobble boards, and balancing pads.
- Functional exercises and sport-specific drills to enhance dynamic stability during intricate motions.
6. Advanced Physiotherapy Modalities
- Capacitive-Resistive Energy Transfer (C.R.E.T.) therapy: A non-invasive method that enhances tissue circulation and oxygenation, decreases inflammation, and speeds up recovery.
- Shock Wave Therapy: Encourages soft tissue healing, increases blood flow, and dissolves calcifications.
- The Super Inductive System (SIS): Uses high-frequency electromagnetic stimulation to help with pain alleviation and muscular strengthening.
7. Functional Rehabilitation
- Including lunges, step-ups, and squats while paying close attention to proper patellar monitoring.
- A gradual return to dynamic exercises, such as jumping and sideways motions, to maintain control and alignment when doing sports-specific duties.
8. Patellar Stabilization Techniques
- Taping: To offer support and adjust patellar alignment, use McConnell or kinesiology taping techniques.
- Bracing: Personalized patellar braces to reduce excessive movement and boost self-assurance while engaging in exercises.
9. Patient Education
- Education on good posture, movement patterns, and biomechanics to reduce excessive knee strain.
- Recurrence prevention guidelines for safe sports and activity participation.
Surgical Management
Recurrent instability, severe anatomical anomalies, or the failure of conservative therapy may all require surgery. Typical procedures consist of:
- MPFL Reconstruction: Rebuilding the ligament to stop the patella from moving laterally is known as MPFL reconstruction.
- Trochleoplasty: When a patient’s trochlea is flat, the trochlear groove is deepened.
- Tibial Tubercle Transfer: Patellar tendon realignment for proper tracking.
- Lateral Release: Reducing patellar tilt by cutting tight lateral structures.
When surgery is necessary, Elite Physiotherapy and Sports Injury Centre will work post-operative management to provide a smooth transition from surgery to recovery.
At Elite Physiotherapy and Sports Injury Centre, we incorporate these therapies into a comprehensive treatment program that is tailored to each patient’s specific requirements. Our blend of state-of-the-art modalities and evidence-based practices guarantees the best possible recovery and long-term avoidance of patellofemoral instability.