Introduction
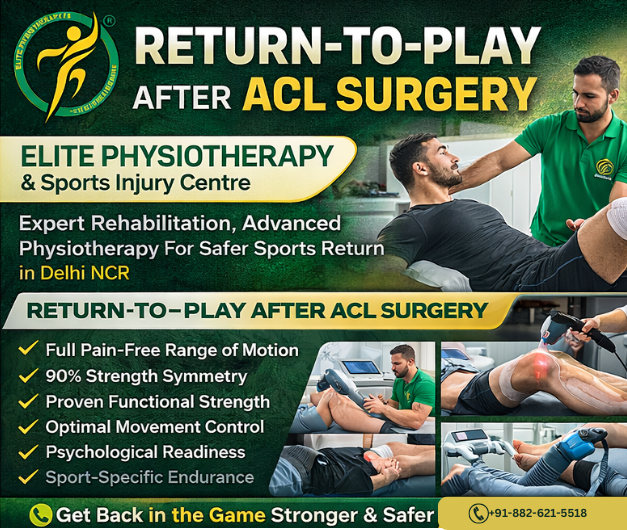
- Athletes and active people frequently have anterior cruciate ligament injuries. Surgery by itself, however, does not ensure a safe return to sports. Return-to-Play Requirements: There is a methodical decision-making process following ACL surgery. It guarantees that before the competition, the athlete regains strength, stability, and confidence.
- Movement quality, performance readiness, and scientific rehabilitation are our main priorities at Elite Physiotherapy and Sports Injury Centre. Our cutting-edge physiotherapy method in Delhi NCR lowers the chance of reinjury and helps athletes return to their best.
- The objective is straightforward. Make a stronger, safer, and more intelligent return.
What is ACL Surgery Rehabilitation?
- ACL restoration uses a graft to replace the damaged ligament. Knee function is then gradually restored through rehabilitation.
- Return-to-Play Criteria After ACL Surgery refers to meeting specific functional and physical requirements before engaging in sports.
- Readiness is not just determined by time. Functional recovery does.
Causes of ACL Injury
- Sudden direction change
- Improper landing mechanics
- Knee valgus collapse
- Weak hip and core muscles
- Poor neuromuscular control
- Previous knee injury
- Athletes in football, wrestling, basketball, and badminton face a higher risk.
Types of ACL Reconstruction
- Classification depends on graft selection:
- Hamstring tendon graft
- Patellar tendon graft
- Quadriceps tendon graft
- Allograft reconstruction
- Each type requires a slightly modified physiotherapy progression.
Clinical Features After ACL Surgery
- Patients may experience:
- Knee swelling
- Quadriceps weakness
- Reduced range of motion
- Instability feeling
- Pain during loading
- Fear of movement
- Therefore, structured Return-to-Play Criteria After ACL Surgery becomes essential.
Diagnostic Evaluation and Examination
- A detailed assessment guides rehabilitation progression.
- Clinical Examination Includes:
- Range of motion assessment
- Swelling evaluation
- Muscle strength testing
- Movement analysis
- Functional performance testing
Assessment Techniques for Return-to-Play
At Elite Physiotherapy, assessment remains objective and measurable.
1. Strength Testing
- Quadriceps and hamstring strength should reach at least 90% symmetry compared to the opposite limb.
2. Functional Hop Tests
- Single hop for distance
- Triple hop test
- Crossover hop test
- Timed hop test
- Poor symmetry indicates incomplete recovery.
3. Movement Quality Analysis
- Psychological Readiness
Physiotherapy Management
- Physiotherapy forms the foundation of Return-to-Play Criteria After ACL Surgery. Rehabilitation progresses through phases.
Phase 1: Protection and Activation
- Early physiotherapy focuses on swelling reduction and mobility.
- Treatment includes:
- Cryotherapy
- Patellar mobilization
- Gentle range exercises
- Quadriceps activation drills
- Gait correction training
- Early muscle activation prevents long-term weakness.
Phase 2: Strength Restoration
- Once pain reduces, progressive strengthening begins.
- Key exercises:
- Closed chain strengthening
- Controlled squats
- Step-ups
- Hip and core stability training
- At our physiotherapy facility in Saket & gurugram, movement quality takes priority over load.
Phase 3: Neuromuscular Control
- This phase rebuilds coordination and joint awareness.
- Training includes:
- Balance training
- Proprioceptive drills
- Perturbation exercises
- Single-leg stability work
- These exercises prepare the knee for unpredictable sports movements.
Phase 4: Power and Plyometric Training
- Athletes begin explosive training gradually.
- Programs include:
- Jump mechanics correction
- Deceleration drills
- Agility ladder work
- Sport-specific movement retraining
- This stage strongly influences the Return-to-Play Criteria After ACL Surgery success.
Phase 5: Sports Reintegration
- Final physiotherapy focuses on performance.
- We introduce:
- Cutting drills
- Sprint progression
- Reaction training
- Match simulation exercises
- Athletes must pass objective testing before clearance.
Role of Advanced Physiotherapy Modalities
- Shock Wave Therapy
- Improves tissue healing and reduces persistent tendon pain around the knee.
- Super Inductive System (SIS)
- Enhances neuromuscular activation. It improves quadriceps recruitment safely.
- High Intensity Laser Therapy
- Reduces inflammation and promotes deep tissue repair.
- Dry Needling and Cupping
- Relieves muscle tightness and improves circulation. These methods reduce compensatory movement patterns.
- These modalities support faster and safer rehabilitation when combined with exercise therapy.
Key Return-to-Play Criteria After ACL Surgery
- Athletes must achieve:
- Full pain-free range of motion
- Minimal swelling
- Strength symmetry above 90%
- Proper landing mechanics
- Successful hop test performance
- Psychological readiness
- Sport-specific endurance
- Meeting all criteria lowers reinjury risk significantly.
Why Choose Elite Physiotherapy and Sports Injury Centre?
- We deliver evidence-based physiotherapy near me solutions across Delhi NCR.
- Our approach includes:
- Personalized rehabilitation programs
- Athlete-specific return protocols
- Advanced technology modalities
- Performance testing systems
- Injury prevention education
- At Elite, we do not rush returns. We prepare athletes for long careers.
Conclusion
- It’s not a race to recover from an ACL. It is a methodical process.
- Athletes can return to play with confidence and safety thanks to the Return-to-Play Criteria following ACL surgery. Effective physiotherapy turns recovery into improved performance.
- Elite Physiotherapy and Sports Injury Centre is prepared to assist you in becoming an excellent athlete once more if you require skilled ACL rehabilitation in Delhi NCR.